Carotid Aneurysm
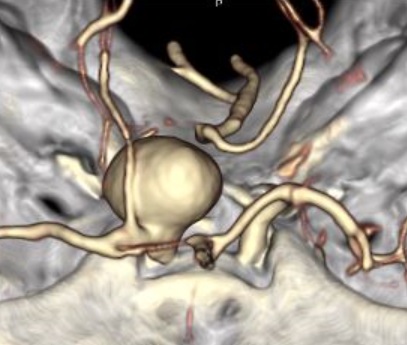
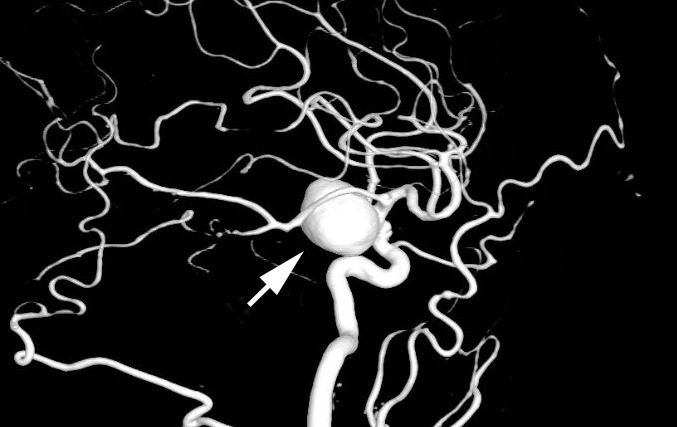
- Ballooning of an unruptured segment of the intracranial internal carotid artery because of a vascular wall defect (“saccular aneurysm,” “berry aneurysm”)
- Congenital defect in the vessel wall is worsened by arteriosclerosis, hypertension, smoking
- Located at the internal carotid–ophthalmic artery junction or more distally on the supraclinoid internal carotid segment
- Vision loss occurs by compression of the optic nerve or chiasm by an enlarging unruptured aneurysm
- More distal aneurysm at the junction of the posterior communicating artery typically causes an ipsilateral third nerve palsy (See Third Nerve Palsy )
-
Core clinical features
- Slowly progressive visual loss in one eye or both, although sudden enlargement of an aneurysm can produce acute vision loss
- Visual acuity is normal or decreased
- Nerve fiber bundle or hemianopic visual field defects
- Afferent pupil defect
- Normal-appearing or pale optic discs
-
Possible accompanying clinical features
- Headache
- Hypopituitarism
- Ipsilateral third nerve palsy
-
Imaging features
- Brain CT or MRI shows a mass in the middle fossa
- CT or MR angiography confirms the diagnosis
- Digital angiography defines the lesion

- Other intracranial tumors
- Optic neuritis
- Neuromyelitis optica
- Lymphocytic hypophysitis
- Sarcoidosis
- Metastatic cancer
- Langerhans cell histiocytosis
- Order brain CT or MRI in any patient with unexplained retrobulbar vision loss
- Order brain CTA or MRA if you suspect aneurysm from CT or MRI
- Refer to an interventionalist for clipping, coiling, stent-coiling, or a flow-diverting stent
-
Without intervention, rupture rates are based mostly on the cross-sectional diameter of the aneurysm
- <7mm: negligible
- ≥7mm but <13mm: 1/2% per year
- ≥13mm to <25mm: 3% per year
- ≥25mm (“giant aneurysm”): 8% per year
- Intervention is usually reserved for aneurysms of greater than 7mm cross-sectional diameter
- Coiling has the lowest morbidity, but coiling alone may not be safe in wide-necked aneurysms because of coil migration into the parent artery, in which case a stent may be added
-
Trap: coiling-induced aneurysm expansion or sac wall inflammation may exacerbate vision loss
- Clipping has a low risk of aneurysm recurrence, but peri-operative morbidity is higher than with coiling
- Flow diversion with a non-fenestrated stent may be sufficient to prevent aneurysm rupture
- Choice and risks of intervention depend on the experience of the interventionalist, the features of the aneurysm, and the age and health of the patient
