Arteritic Ischemic Optic Neuropathy
- Infarction of the optic disc caused by inflammatory occlusion of branches of the ophthalmic artery
- Giant cell (temporal) arteritis is the principal underlying condition
- Affects patients 60 years or older
- Diagnosis is suggested by a combination of ophthalmic, constitutional, and laboratory abnormalities
- Diagnosis is confirmed by temporal artery biopsy showing characteristic vessel wall signs
- Prompt high-dose corticosteroid treatment reduces the chances of fellow eye involvement
-
Core features
- Acute painless monocular or binocular vision loss
- Reduced visual acuity, nerve fiber bundle visual field defects
- Afferent pupil defect in the affected eye unless vision loss is equal in both eyes
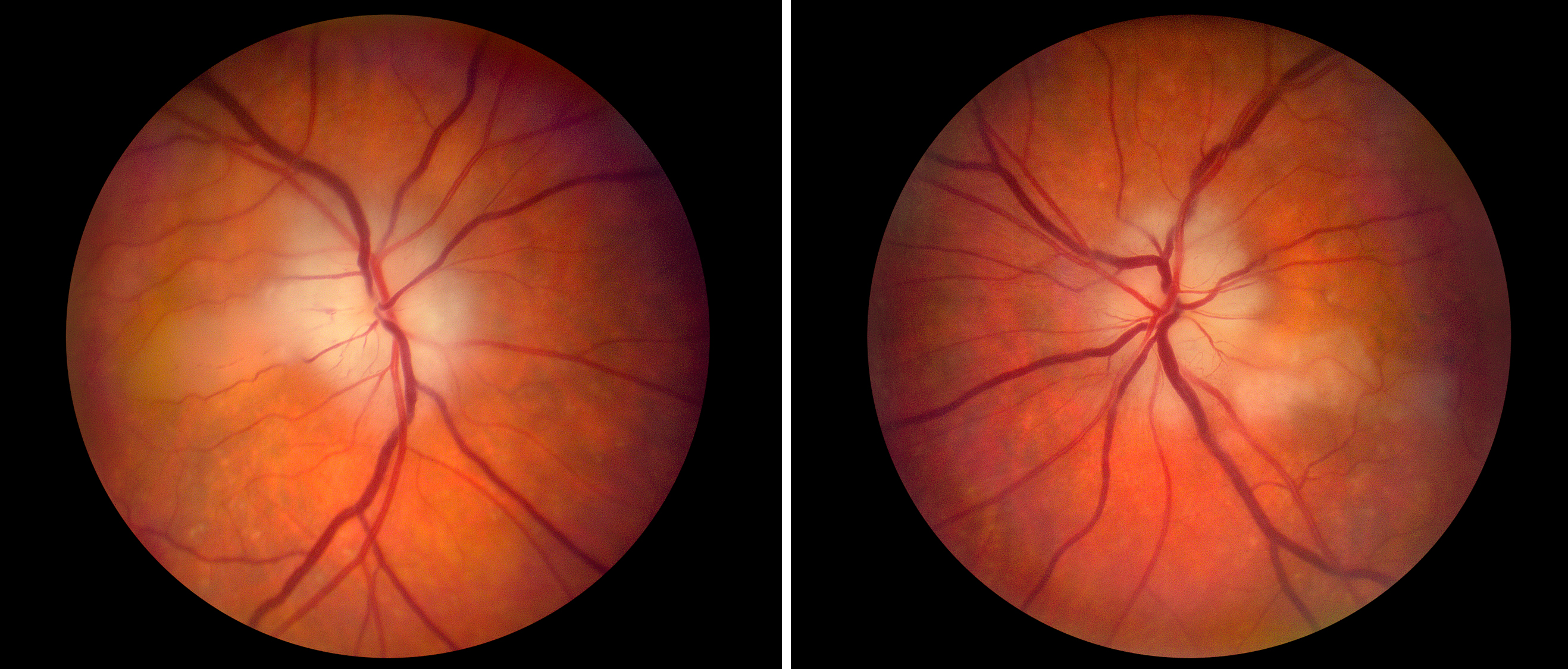
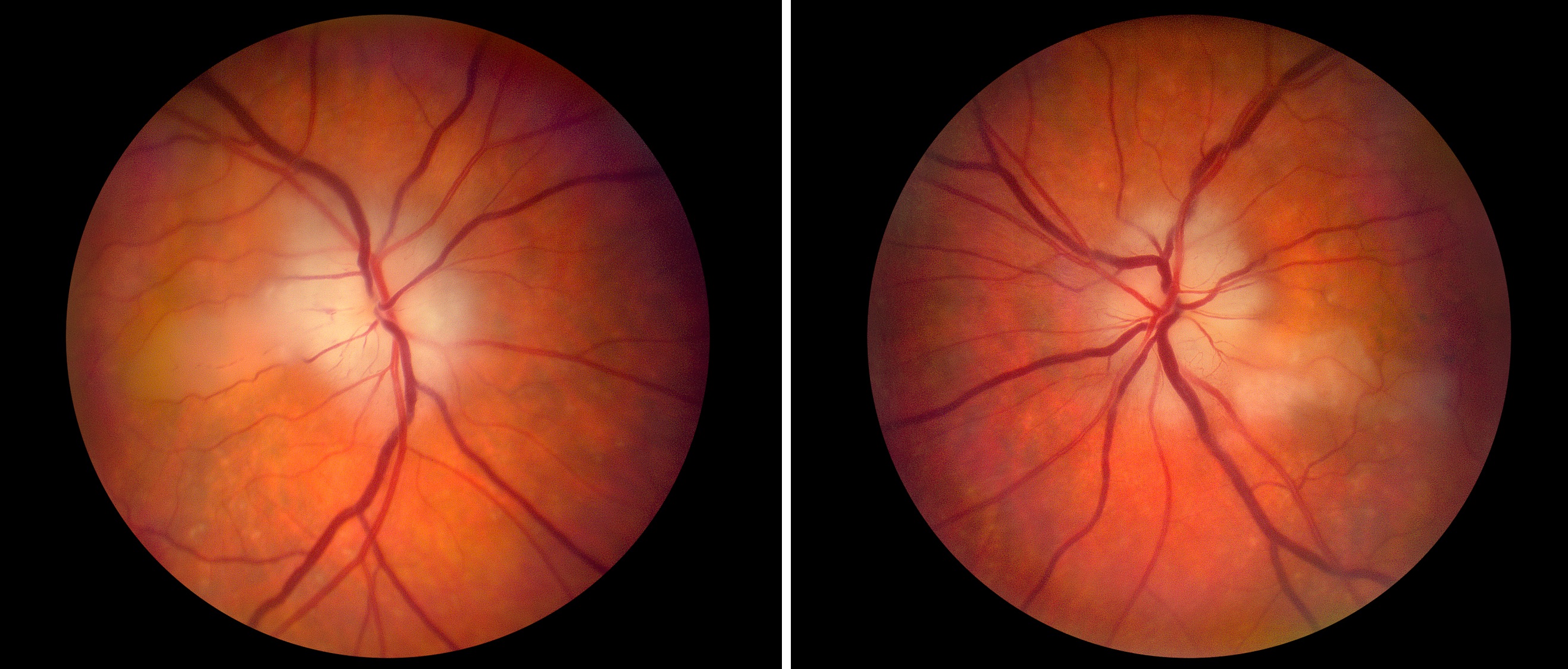
- Acquired optic disc elevation--often pallid with hemorrhage--in >95%
-
Tip: the absence of optic disc edema does not exclude—but casts doubt on--this diagnosis
-
Possible accompanying ophthalmic features
- Retinal artery occlusion, cotton wool spots
- Choroidal ischemia
- Anterior chamber flare, lens opacity, ocular hypotony (“ocular ischemic syndrome”)
- Diplopia from extraocular muscle ischemia or ocular motor palsy
-
Possible accompanying systemic features
- New headache
- Scalp tenderness
- Deep jaw ache with chewing (jaw claudication)
- Fatigue, anorexia, limb girdle aches (polymyalgia rheumatica symptom complex)
-
Possible imaging features
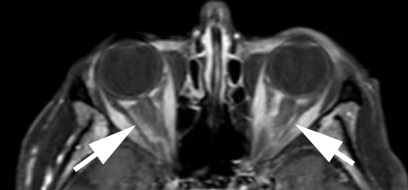
- MRI enhancement of the retrobulbar optic nerve, dura, and/or orbital soft tissues
-
Tip: polymyalgia rheumatica often pre-exists, but its symptoms may be so chronic and subtle as to recognized only in retrospect
-
Tip: patients are eligible for this diagnosis even without ANY systemic symptoms
- Non-arteritic ischemic optic neuropathy
- Papillitis
- Atypical optic neuritis
- Hypotensive ischemic optic neuropathy
- Papilledema
- Central retinal vein occlusion
- Infiltrative (neoplastic) optic neuropathy
-
If the erythrocyte sedimentation rate and C-reactive protein are elevated and/or clinical findings suggest giant cell arteritis
- Treat promptly with intravenous methylprednisolone 1g/day for 3-5 days or the oral equivalent, followed by prednisone 1mg/kg/day
- Perform unilateral temporal artery biopsy within 2 weeks of starting corticosteroids, harvesting at least 2 cm of artery
-
Send the biopsy to an experienced pathologist, who will find one or more of the following abnormalities in 96% of specimens

- Thickening and inflammatory destruction of the vascular media–intima junction
- Fragmentation of the internal elastic lamina
- Langerhans giant cells
-
Trap: the pathologist may miss pertinent abnormalities unless a wide extent of artery is examined because the lesions may be discontinuous (skip lesions)
-
Trap: fibrosis (scarring) without inflammation of the vessel wall, which has been called “healed arteritis,” is no longer considered diagnostic of giant cell arteritis
- Advise the pathologist to hunt for a scarred vessel wall and fragmentation of the internal elastic lamina (healed arteritis) if the biopsy is performed more than 2 weeks after corticosteroid treatment is started
-
If the biopsy is positive
- Taper oral prednisone at 10mg/week, reaching a prednisone dose of 10mg/day by 8 weeks after diagnosis
- When 8 weeks have elapsed since diagnosis, raise the prednisone dose only if the patient redevelops symptoms suggesting active disease, disregarding elevation of the sedimentation rate and/or C-reactive protein unless dramatic
-
Trap: raising the prednisone dose based on rebound elevation of the sedimentation rate or C-reactive protein after 8 weeks have elapsed since diagnosis invites corticosteroid complications and does not reduce the chance of visual loss
- Keep the daily prednisone dose at a minimum of 10mg/day for 1 year
- Tocilizumab (Actemra) can be used to allow more rapid tapering of corticosteroid and to reduce long term corticosteroid complications, but…
-
Trap: do not use tocilizumab in place of corticosteroids initially, as its anti-inflammatory effects take time to develop
-
If the biopsy is negative
- Stop corticosteroid treatment and diagnose non-arteritic ischemic optic neuropathy unless…
- Clinical findings strongly suggest arteritis or fluorescein angiography shows choroidal filling defects, in which case…
- Perform temporal artery biopsy on the other side, but expect a different result in fewer than 10% of rebiopsies
- If all studies are negative, continue treatment only if clinical evidence for arteritis is overwhelming
- Visual loss usually remains stable in the affected eye, but may worsen
- Ischemic optic neuropathy may strike the fellow eye despite treatment
- Corticosteroid treatment should be continued no longer than 18 months after diagnosis because the risk of reactivation is very low by that time and complications of prolonged corticosteroid use become unacceptably high