( of )
Correct: 0
Incorrect: 0
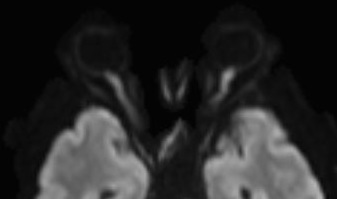
A 55 year old man undergoes multilevel lumbar spine surgery for spinal stenosis and awakens with impaired vision in both eyes. He had a thorough and normal pre-operative optometric examination 1 month before surgery. Visual acuity now is 20/100 (6/30, 0.2) in both eyes. There is an afferent pupil defect in the right eye. Intraocular pressures are normal. Visual fields appear normal at the bedside, and the optic fundus, through clear media, appears normal. This is a diffusion-weighted axial MRI scan.
What caused the vision loss?
Correct!
The diffusion-weighted MRI is showing increased signal in both optic nerves, an indication of recent infarction. The cause was probably intra-operative
systemic hypotension, which sometimes occurs accidentally or deliberately (to reduce hemorrhage that interferes with the surgeon’s view in the operative field).
Called “peri-operative ischemic optic neuropathy” or “hypotensive ischemic optic neuropathy,” its mechanism is believed to be lack of perfusion of the intra-orbital
optic nerve. The patient usually notices the vision loss upon regaining full consciousness, although it may initially be attributed to sedating analgesics. The
radiologist’s attention should be drawn to the optic nerves and diffusion-weighted imaging should be included in the MRI study. Maintaining normal
post-operative blood pressure is a reasonable gesture. Hyperbaric oxygen treatment and corticosteroids, often proposed, are not effective. Vision may
spontaneously improve somewhat if the infarction has not been severe.
Bilateral optic neuritis is not a favored diagnostic choice in this setting. Pituitary apoplexy can certainly occur in systemic hypotension, but you might expect to see a bitemporal hemianopia on visual field examination and anyway, the imaging abnormality here lies in the optic nerves, not the optic chiasm. And yes, visual cortex infarction can certainly occur in this setting, but the afferent pupil defect points to an optic nerve localization.
Bilateral optic neuritis is not a favored diagnostic choice in this setting. Pituitary apoplexy can certainly occur in systemic hypotension, but you might expect to see a bitemporal hemianopia on visual field examination and anyway, the imaging abnormality here lies in the optic nerves, not the optic chiasm. And yes, visual cortex infarction can certainly occur in this setting, but the afferent pupil defect points to an optic nerve localization.
Incorrect
Incorrect
Incorrect