( of )
Correct: 0
Incorrect: 0
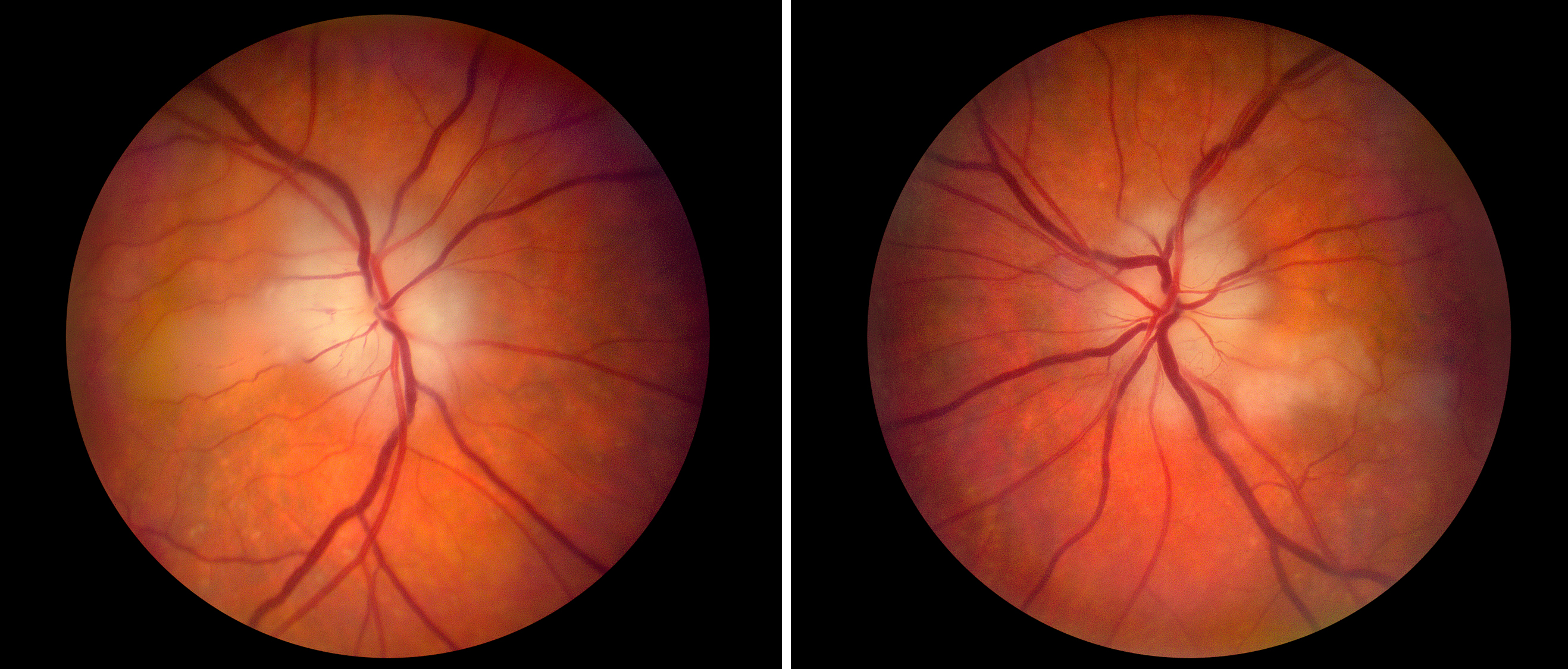
A 70 year old woman reports loss of vision in both eyes over the previous weekend. She has been taking a nonsteroidal anti-inflammatory (NSAID) medication for “arthritis” but has otherwise been free of health concerns. Visual acuities are reduced to finger counting in both eyes. There is no afferent pupil defect. Acute phase reactants (erythrocyte sedimentation rate, C-reactive protein) are normal. Here is the appearance of the optic fundi.
You should order
Incorrect
Incorrect
Correct!
 Bilateral simultaneous optic disc swelling often prompts consideration of papilledema from increased intracranial pressure, but papilledema does not usually
cause such severe vision loss acutely. Moreover, the optic disc swelling here is pallid, therefore likely ischemic. Yes, she lacks systemic manifestations of
giant cell arteritis, but the NSAID medication may be masking them! She does not have elevated acute phase reactants, but the fact that both optic discs are
affected SIMULTANEOUSLY nearly excludes non-arteritic ischemic optic neuropathy and demands prompt exclusion of giant cell arteritis (GCA). Therefore, she must
undergo immediate corticosteroid treatment to help protect her against further visual and nonvisual deficits, followed by temporal artery biopsy as soon as
possible.
Bilateral simultaneous optic disc swelling often prompts consideration of papilledema from increased intracranial pressure, but papilledema does not usually
cause such severe vision loss acutely. Moreover, the optic disc swelling here is pallid, therefore likely ischemic. Yes, she lacks systemic manifestations of
giant cell arteritis, but the NSAID medication may be masking them! She does not have elevated acute phase reactants, but the fact that both optic discs are
affected SIMULTANEOUSLY nearly excludes non-arteritic ischemic optic neuropathy and demands prompt exclusion of giant cell arteritis (GCA). Therefore, she must
undergo immediate corticosteroid treatment to help protect her against further visual and nonvisual deficits, followed by temporal artery biopsy as soon as
possible.
The pathologist will be looking for thickening and inflammatory destruction of the vascular media–intima junction
fragmentation of the internal elastic lamina
and/or Langerhans giant cells
If biopsy of one side is negative, you should consider biopsy of the other side, which improves the detection rate of giant cell arteritis from 93% to 96%.
Were a double biopsy to be negative, you would be in a quandary. Make sure that the specimens are of adequate length (at least 2cm) and carefully reviewed by
an expert.
If the biopsy is certifiably negative, some authorities might suggest a temporal artery Duplex color ultrasound, looking for hypoechoic vascular thickening, or a high-resolution temporal artery MRI, looking for enhancement and wall thickening. If positive, those results would trump the negative temporal artery biopsy and justify intensive treatment. Fluorescein angiography might be useful to detect choroidal ischemia, a feature of giant cell arteritis, but its sensitivity is low. Optic coherence tomography contributes nothing here. Brain/orbit MRI is being increasingly ordered in suspected GCA because it may show inflammatory changes in the perioptic dura and orbital fat, findings not expected in non-arteritic ischemic optic neuropathy.

The pathologist will be looking for thickening and inflammatory destruction of the vascular media–intima junction
If the biopsy is certifiably negative, some authorities might suggest a temporal artery Duplex color ultrasound, looking for hypoechoic vascular thickening, or a high-resolution temporal artery MRI, looking for enhancement and wall thickening. If positive, those results would trump the negative temporal artery biopsy and justify intensive treatment. Fluorescein angiography might be useful to detect choroidal ischemia, a feature of giant cell arteritis, but its sensitivity is low. Optic coherence tomography contributes nothing here. Brain/orbit MRI is being increasingly ordered in suspected GCA because it may show inflammatory changes in the perioptic dura and orbital fat, findings not expected in non-arteritic ischemic optic neuropathy.