( of )
Correct: 0
Incorrect: 0
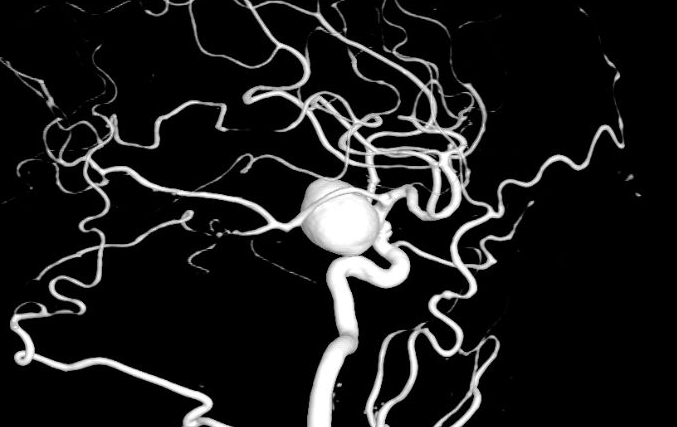
A 65 year old man is found on routine optometric examination to have reduced visual acuity in the right eye and a temporal hemianopic defect in the left eye on formal visual field examination. There is a right afferent pupil defect and the right optic disc is pale. Otherwise the optometric examination is normal. A heavy smoker, he is being treated for systemic hypertension. Imaging shows this aneurysm, which measured 25mm in diameter.
If untreated, what chance is there that the aneurysm will rupture?
Incorrect
Incorrect
Incorrect
Correct!
The pattern of vision loss described here—reduced visual acuity and afferent pupil defect in one eye and a temporal hemianopic visual field defect in the
other eye—localizes to the optic nerve-optic chiasm junction. Mass lesions are usually responsible. The most common ones are pituitary adenomas, meningiomas,
craniopharyngiomas, and pilocytic astrocytomas, but aneurysms are not far behind. This giant aneurysm is probably arising from the supraclinoid internal carotid
artery. Studies have established an 8% per year rupture rate, with a 50% mortality rate. Fortunately, aneurysms can be prevented from rupturing by clipping
them at their necks, placing coils within them that promote clotting, and by diverting arterial blood flow with stents. Admittedly, such interventions carry risks
of stroke and intra-procedural aneurysm rupture. But some type of aneurysm repair should take place unless the patient is too sick to be a candidate.
Of all the possible causes of this pattern of vision loss, aneurysm is the most feared because of the threat of rupture and instant death. For that reason, patients with these presenting visual features must undergo relatively prompt retrobulbar imaging, including sequences that adequately visualize blood vessels.
Of all the possible causes of this pattern of vision loss, aneurysm is the most feared because of the threat of rupture and instant death. For that reason, patients with these presenting visual features must undergo relatively prompt retrobulbar imaging, including sequences that adequately visualize blood vessels.