Eye Movement Examination
-
Assess fixation
- Patient fixates on your stationary light or finger
- Look for spontaneous eye movements that take the eyes off fixation
-
Assess ocular pursuit
- Patient follows your moving finger or light in all gaze directions
- Note the amplitude and smoothness of eye movements and look for oscillations in extremes of gaze
-
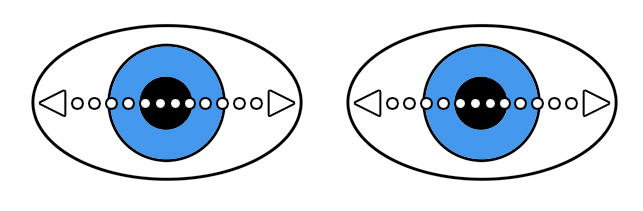
Assess saccades
- Patient looks sequentially to the right, left, up, and down at your stationary light or finger displayed eccentrically
- Note the latency, speed, and accuracy of eye movements
-
Assess vestibulo-ocular reflex (VOR)
- If ocular pursuit and saccades are deficient, rotate the patient’s head slowly back and forth horizontally and vertically (“Doll’s eye maneuver”)
- Look for slow conjugate eye movements in the direction opposite to head movement
- If saccades and pursuit appear intact, but the patient reports blurred vision or oscillopsia with head movement, perform the following
-
Head impulse test
- Grasp the patient’s head and move it briskly horizontally to the right and then to the left, looking for corrective versional saccades opposite in direction to head movement
-
Dynamic visual acuity test
- Instruct the patient to read the smallest identifiable line on the Snellen chart without head movement
- Move the patient’s head briskly back and forth, looking for a decline in visual acuity relative to that achieved with the head immobile
-
Perform occlusive direct ophthalmoscopy to evoke nystagmus caused by a peripheral vestibular lesion
- During direct ophthalmoscopy, look for oscillations of the optic fundus
- Cover the unexamined eye and note whether you have evoked or increased the amplitude of oscillations in the eye you are examining with the ophthalmoscope
-
Perform the optokinetic nystagmus test
- Hold the optokinetic strip or drum at reading distance and rotate it in the horizontal plane to the right and then to the left; then rotate the strip or drum in the vertical plane, first upward, then downward
- Note the amplitude of evoked nystagmus
-
Perform the Dix-Hallpike (Nylen-Barany) maneuver in a patient who reports positional vertigo
- Grasp the patient’s head and carry the patient from a sitting to a supine position, lowering the head over the edge of the examining table, first with the head positioned straight down, then with the head moved to the right and to the left
- Note any evoked nystagmus
-
Order the caloric irrigation test if you need a more sensitive test of vestibulo-ocular function
- Performed only in the vestibular laboratory
- Patient is placed in the supine position with the head elevated 30 degrees
- Tympanum is inspected to make sure it is intact
- Cold water is instilled into the external ear canal
- Eye movements are recorded, usually with video goggles
-
Tip: if volitional movement (pursuit, saccades) is reduced in one eye or asymmetrically reduced between the two eyes, expect one of these possible causes
-
extraocular muscle weakness, scarring, or cramp
-
an orbital lesion that obstructs movement of the eye
-
neuromuscular transmission failure (usually myasthenia gravis)
-
ocular motor (third, fourth, or sixth) cranial nerve damage
-
internuclear ophthalmoplegia
-
-
Tip: if volitional movement (pursuit, saccades) is symmetrically reduced in both eyes, the damage probably affects the central nervous system control of eye movements
-
Impaired fixation
- Spontaneous movements of the eyes away from fixation indicate inattention, nystagmus, or saccadic intrusions
-
Binocularly symmetrical impairment of pursuit
- Jerky (“saccadic,” “cogwheel”) pursuit indicates central nervous dysfunction, but is not localizing
-
Trap: pursuit will appear jerky if the patient is inattentive, uncooperative, or obliged to follow a target moving faster than 30 degrees/second
-
Binocularly symmetrical impairment of saccades
- Slow, delayed, reduced, or inaccurate saccades derive from many kinds of central nervous system disorders
- Unidirectional deficit of saccades suggests brain stem dysfunction
-
Binocularly symmetrical impairment of saccades and pursuit but an intact vestibulo-ocular reflex
- If congenital and accompanied by head thrusts, suggests congenital ocular motor apraxia
- If acquired and chronic, suggests progressive supranuclear palsy
- If acquired and acute, suggests acquired ocular motor apraxia from bilateral cerebral hemispheric ischemia
-
Abnormal head impulse test
- Conjugate refixational saccades opposite in direction from brisk head movement suggest an impaired vestibulo-ocular reflex
- If the head impulse test is positive only in one direction, consider a diagnosis of unilateral peripheral vestibulopathy
- If the head impulse test is positive in both directions, consider a diagnosis of bilateral peripheral vestibulopathy
-
Abnormal dynamic visual acuity test
- Visual acuity decline of at least 2 Snellen lines with head motion suggests a bilateral peripheral vestibulopathy
-
Abnormal occlusive direct ophthalmoscopy
- Nystagmus that develops or worsens after covering the unexamined eye suggests a peripheral vestibulopathy
-
Abnormal optokinetic nystagmus test
- Convergence retraction eye movements evoked by downwardly moving stripes suggest dorsal midbrain dysfunction
- Relatively reduced nystagmus amplitude of one eye suggests reduced innervation of the extraocular muscle normally recruited in the direction of the fast phase of nystagmus
- Jerk nystagmus with its fast phase in the direction of the moving stripes suggests infantile nystagmus syndrome (“reversal of optokinetic nystagmus”)
- Relatively reduced conjugate horizontal nystagmus amplitude in one gaze direction suggests an ipsilateral parietal lesion
- Lack of any evoked nystagmus suggests organic vision loss or marked inattention
-
Abnormal Dix-Hallpike (Nylen-Barany) maneuver
- Upbeat torsional nystagmus with its fast phase toward the dependent ear suggests posterior semicircular canal benign positional vertigo
- Downbeat nystagmus suggests cerebellar disease
- Other nystagmus patterns do not differentiate between brainstem, end-organ, and vestibular nerve dysfunction
-
Abnormal caloric irrigation test
- Lack of evoked horizontal conjugate eye movement indicates severe dysfunction of the brainstem or both vestibular nerves
- Relatively reduced amplitude of oppositely-directed jerk nystagmus indicates labyrinthine or vestibular nerve dysfunction on the side of the reduced nystagmus amplitude