Dorsolateral Medullary (Wallenberg) Syndrome
- Core neuro-ophthalmic features
-
Possible accompanying neurologic features
- Ipsilateral extremity and gait ataxia
- Nausea and vomiting
- Hoarseness, swallowing difficulty, intractable hiccups
- Ipsilateral facial numbness (trigeminal hypesthesia)
- Contralateral extremity numbness (spinothalamic hypesthesia)
- Ataxia
-
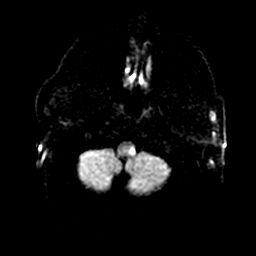
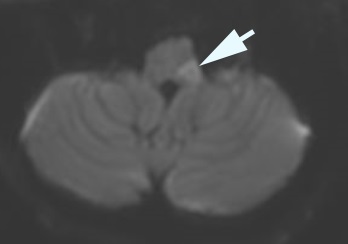
Imaging features
- Restricted diffusion in the dorsolateral medulla and/or inferolateral cerebellar hemisphere
- Blood in the wall of the vertebral artery
- Narrowing or occlusion of the ipsilateral vertebral artery
- If other neurologic deficits are present, diagnose a cerebellar or more rostral brainstem lesion, or multiple lesions
-
Look for the following combination of signs as unique to Wallenberg syndrome
- Skew deviation
- Horner syndrome
- Nystagmus
- Ataxia
- Difficulty swallowing
- Intractable hiccups (singultus)
- Numbness (hypesthesia) on the ipsilateral face and contralateral extremities
-
Tip: order immediate brain CT/CTA (and MRI/MRA if CT/CTA is unrevealing) to rule out vertebral artery dissection, cerebellar infarction, or cerebellar hemorrhage, because cerebellar swelling could threaten medullary function, warranting emergency neurosurgical decompression to prevent death
- Monitor intensively for the first 48 hours for declining brainstem function
-
Tip: anticoagulation has not been shown to be superior to aspirin in preventing further stroke
-
Consider these other interventions
- Prism or ocular occlusion for palliation of diplopia
- Medicinal palliation of vertigo, intractable nausea and vomiting, hiccups
- Nasogastric intubation for swallowing difficulty and to prevent aspiration
- Physical therapy for ataxia
- Substantial recovery usually occurs, but may be delayed for months
-
Tip: marked clinical manifestations and cerebellar involvement on MRI are associated with early clinical decline and a longer duration of deficits
- Nausea, vertigo, hiccups may be severe for weeks
- Diplopia, Horner syndrome, and ataxia often endure indefinitely