Acute Comitant Esotropia
- Recent-onset diplopia and comitant esotropia when fixating a distant target
- Full ocular versions and ductions
- Common causes: accommodative esotropia, breakdown of latent esophoria, spasm of the near reflex, high myopia
- Uncommon (but serious) causes: increased intracranial pressure, subarachnoid hemorrhage, acute thalamic or brainstem lesion, meningoencephalitis
- Core neuro-ophthalmic features
- Possible accompanying neuro-ophthalmic features
-
Possible other accompanying features
- Hyperopic refractive error
- Headache
- Ear pain
- Reduced consciousness
- Impaired cognition
- Ataxia
- Extremity weakness and numbness
-
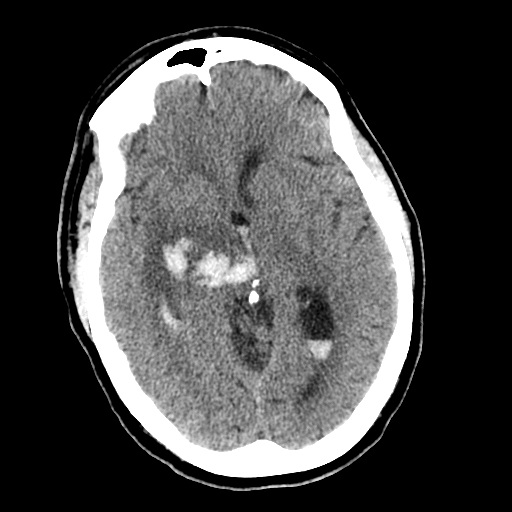
Possible imaging features
- Ventriculomegaly
- Cerebellar, thalamic, or midbrain lesion
- Meningitis
- Subarachnoid hemorrhage
- Dural venous sinus thrombosis
- Lumbar puncture may show an elevated opening pressure or abnormal constituents suggesting meningitis or subarachnoid hemorrhage
- Bilateral sixth nerve palsies, which should be accompanied by incomitant esotropia
- Look for sedative medications that could have caused a decompensated esophoria
-
Look for signs of spasm of the near reflex
- Convergence movements that interrupt ocular versions
- Episodic miosis and pseudomyopia
- Look for an uncorrected hyperopic refractive error
-
Tip: accommodative esotropia rarely has its onset after age 3 and rarely includes diplopia
- Look for high myopia
-
Tip: the esotropia of high myopia may have a subacute onset
- Exclude signs of an underlying brain lesion
- Order brain MRI if you cannot attribute the esotropia to sedative medication, accommodative esotropia, spasm of the near reflex, or high myopia
- Order lumbar puncture if MRI is normal and there are features to suggest a neurologic illness
- Most cases without other neurologic features will be caused by decompensated esophoria, accommodative esotropia, or spasm of the near reflex, but…
-
Tip: distinguishing between decompensated esophoria and spasm of near reflex may be difficult
- Accommodative esotropia can be corrected with the appropriate hyperopic glasses prescription
- Diplopia of decompensated esophoria is easily palliated with base-out prism
-
Eye muscle surgery is indicated only if
- Esotropia has not resolved after at least 9 months
- Esotropia is large
- Patient does not want to wear glasses with prism
-
Trap: eye muscle surgery for spasm of the near reflex carries a risk of consecutive exotropia (See Spasm of Near Reflex )