( of )
Correct: 0
Incorrect: 0
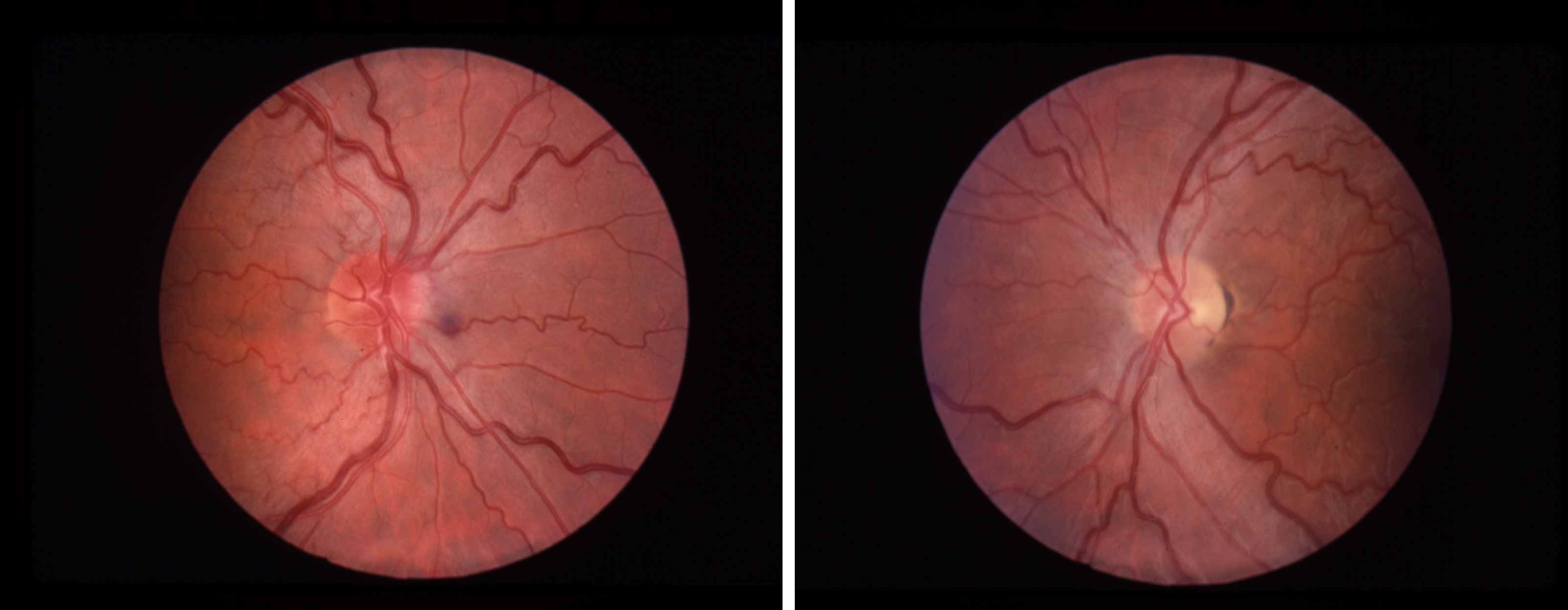
Four months ago, a 22 year old man suffered loss of vision in the left eye over a few days. Examination then showed a slightly swollen left optic disc, a left afferent pupil defect, and a left centrocecal scotoma. Examination of the right eye was normal. There were no systemic or neurologic symptoms. Brain/orbit imaging was negative. Vision did not recover. It was attributed to optic neuritis. Two days prior to his visit to you, he reports that he began to lose vision in his right eye. He admits to heavy alcohol intake at a college party in the week before the visit. Your examination shows a best-corrected visual acuity of 20/100 in each eye. Visual fields now show bilateral centrocecal scotomas. There is no afferent pupil defect. The optic fundus is as you see it here.
What has caused the vision loss?
Incorrect
Incorrect
Incorrect
Correct!
When you encounter a young man with unilateral optic neuropathy and no recovery of vision and normal adequate brain imaging, you must always think of Leber
hereditary optic neuropathy (LHON), a mitochondrial DNA disorder that causes metabolic destruction of retinal ganglion cells that primarily serve visual
acuity.
Confirmed by analysis of blood samples for mutations at specific mitochondrial DNA positions, LHON becomes the prime suspect when the same process strikes the second eye within weeks to months and when the following optic fundus abnormalities are present: 1) temporal optic disc pallor months after an attack; and 2) peripapillary nerve fiber layer thickening and hyperemia before and during an attack, as you see here.
During and after the attack on the first eye, you may not see an afferent pupil defect, perhaps because LHON may spare the intrinsically-photoactive retinal ganglion cells, which continue to transmit on behalf of the pupil light reflex. If you happen to be the examiner when the vision fails in the first eye, and you do not find an afferent pupil defect, you may be tempted to diagnose psychogenic vision loss unless you recognize the relatively distinctive optic disc features. Fluorescein angiography will not show leakage because the blood-retinal barrier is intact; the changes reflect axonal swelling from stasis caused by energy failure.
Unfortunately, there is yet no effective treatment for LHON. You would not be faulted for conducting an investigation for treatable causes, but do not go too far before sending off blood for those mutations! Most laboratories screen for the four main LHON mutations, which are believed to account for at least 90% of cases.
Confirmed by analysis of blood samples for mutations at specific mitochondrial DNA positions, LHON becomes the prime suspect when the same process strikes the second eye within weeks to months and when the following optic fundus abnormalities are present: 1) temporal optic disc pallor months after an attack; and 2) peripapillary nerve fiber layer thickening and hyperemia before and during an attack, as you see here.
During and after the attack on the first eye, you may not see an afferent pupil defect, perhaps because LHON may spare the intrinsically-photoactive retinal ganglion cells, which continue to transmit on behalf of the pupil light reflex. If you happen to be the examiner when the vision fails in the first eye, and you do not find an afferent pupil defect, you may be tempted to diagnose psychogenic vision loss unless you recognize the relatively distinctive optic disc features. Fluorescein angiography will not show leakage because the blood-retinal barrier is intact; the changes reflect axonal swelling from stasis caused by energy failure.
Unfortunately, there is yet no effective treatment for LHON. You would not be faulted for conducting an investigation for treatable causes, but do not go too far before sending off blood for those mutations! Most laboratories screen for the four main LHON mutations, which are believed to account for at least 90% of cases.