( of )
Correct: 0
Incorrect: 0
This 55 year old man had a sudden loss of consciousness one week ago. When he regained consciousness, he displayed these eye movements.
Can you locate the lesion?
Correct!
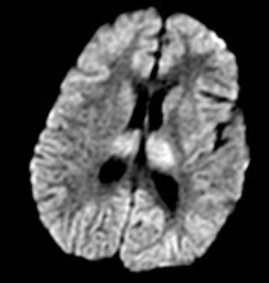
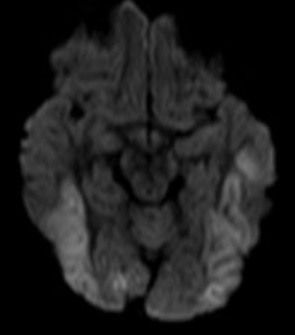 This patient cannot perform voluntary eye movements in any direction. But with passive head movement, the eyes do move somewhat in the opposite direction. This dissociation between
impaired volitional and intact reflex gaze is called a “supranuclear gaze palsy.” As the gaze deficit is in all directions, the lesion must be in both cerebral hemispheres
This patient cannot perform voluntary eye movements in any direction. But with passive head movement, the eyes do move somewhat in the opposite direction. This dissociation between
impaired volitional and intact reflex gaze is called a “supranuclear gaze palsy.” As the gaze deficit is in all directions, the lesion must be in both cerebral hemispheres
or both sides of the thalamus.
Indeed, he had an episode of severe systemic hypotension that caused a lack of perfusion and oxygenation of both cerebral hemispheres. This
phenomenon has been called “acquired ocular motor apraxia,” but the term “apraxia” in this situation is usually reserved for patients who also
have elements of Balint-Holmes syndrome, manifesting as difficulty disengaging from viewed targets and misreaching into extrapersonal space. To
describe the eye movement abnormality, I prefer to use the term “acquired acute supranuclear gaze disorder.” If the supranuclear nature of the ophthalmoplegia is not recognized, the patient may be misdiagnosed as having
myasthenia gravis or polycranial neuropathy. When a supranuclear gaze disturbance develops chronically, the most common cause is progressive supranuclear palsy (PSP). In PSP, vertical
gaze is typically more affected than horizontal gaze, and there will be a parkinsonian state.
Incorrect
Incorrect
Incorrect