Nystagmus Overview
- Involuntary rhythmic oscillation of the eyes initiated by a slow conjugate drift and followed by an oppositely-directed recovery movement
- Called “pendular nystagmus” if the recovery movement is slow
- Called “jerk nystagmus” if the recovery movement is fast
- May be physiologic if the jerk nystagmus is small in amplitude, unsustained, and limited to the extremes of horizontal gaze
- Common causes of pendular nystagmus: diencephalic/brainstem/cerebellar disorder, idiopathic congenital disorder
- Common causes of pathologic jerk nystagmus: medications, acute peripheral vestibulopathy, brainstem/cerebellar disorder, idiopathic congenital disorder
- May be mimicked by saccadic intrusions and other oscillations initiated by a fast eye movement
- Patient may report blurred vision or illusory movement of viewed objects (“oscillopsia”)
- Features of physiologic nystagmus
-
Features of pathologic nystagmus
- Oscillations always begin with a slow conjugate drift
- Oscillations may occur in horizontal, vertical, rotary (torsional), or circular planes
- Oscillations usually involve both eyes, with two notable exceptions:
-
Tip: oscillations may appear monocular in two conditions:
-
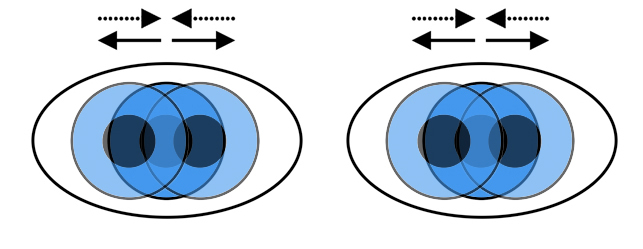
Oscillations are conjugate in most forms of nystagmus, with two notable exceptions:
- Seesaw nystagmus, one eye moves up and intorts while the other eye moves down and extorts, a condition caused by diencephalic or midbrain lesions
- Oculomasticatory myorhythmia, the eyes converge and diverge synchronously with spasms of the masticatory muscles, a condition virtually diagnostic of Whipple disease
- Oscillation fast phase is usually in the direction of gaze, with two notable exceptions:
-
Three common forms of pathologic nystagmus have spectacularly unusual features
- Latent nystagmus: the oscillation amplitude increases when either eye is covered
- Oculopalatal tremor: the oscillations of the eyes, palate, and other branchial arch-derive muscles occur synchronously
- Periodic alternating nystagmus: the direction of the fast recovery phase of horizontal jerk nystagmus switches directions every 2 minutes in primary gaze position
- Square wave jerks: look for binocular unidirectional horizontal saccades followed by a brief interval, and then oppositely-directed saccades that return the eyes to primary gaze position
- Ocular flutter: look for binocular rapid back-to-back horizontal saccades
- Opsoclonus: look for binocular rapid back-to-back horizontal, vertical, and oblique saccades
- Ocular dysmetria: look for back-to-back saccades of decreasing amplitude as the eyes settle on a newly fixated target
- Ocular bobbing: look for conjugate vertical ocular movements with at least one very slow phase in a comatose patient
- Ping pong gaze: look for slow horizontal conjugate movements that take the eyes from one extreme of gaze to the other in a comatose patient
- Step 1: distinguish nystagmus from its imitators, which are NOT initiated by a slow conjugate drift of the eyes, except for ocular bobbing and ping pong gaze, which may have an initial slow conjugate drift but always occur in comatose patients
- Step 2: distinguish physiologic nystagmus from pathologic nystagmus
-
Step 3:
distinguish Infantile nystagmus syndrome by noting these features of the oscillations:
- Begin within the first six months of life
- Usually in the horizontal plane in primary gaze position and remain in the horizontal plane even when the eyes are directed into upgaze or downgaze
- Appear to have a hybrid pendular-jerk waveform (and prove to have an increasing velocity slow phase on eye movement recordings)
- Have reduced amplitude in one eccentric position of gaze (“null zone”)
- Amplitude may be increased by covering one eye (“latent nystagmus”)
- May be accompanied by dissociated vertical deviation or esotropia
- May be accompanied by impaired vision attributable to optic neuropathy, retinopathy, or amblyopia
- May be accompanied by face turn, head tilt, or head titubation
- Step 4: distinguish one form of acquired nystagmus from another by observing the features of the nystagmus and its accompanying features
-
These forms of nystagmus have special diagnostic value
- Monocular abducting nystagmus: usually internuclear ophthalmoplegia, but can be myasthenia gravis
- Seesaw nystagmus: diencephalic lesion, congenital or acquired
- Pure rotary nystagmus: brainstem or diencephalic lesion
- Downbeat nystagmus: medullocerebellar dysfunction, structural or metabolic
- Upbeat nystagmus: diencephalic, brainstem, or cerebellar dysfunction, usually acquired
- Periodic alternating nystagmus: medullocerebellar dysfunction, usually congenital
- Oculopalatal tremor: acquired lesion in Guillain-Mollaret triangle between dentate, olivary, and red nuclei, usually occurring months after a brainstem lesion
- Horizontal nystagmus in primary gaze that remains horizontal in upgaze and downgaze (“uniplanar”): ALWAYS congenital
- Latent nystagmus: ALWAYS congenital
- Purely torsional nystagmus: diencephalic or brainstem/cerebellar dysfunction, usually acquired
- Spasmus nutans: idiopathic but self-limited
- Oculomasticatory myorhythmia: Whipple disease
-
Tip: gaze-evoked sidebeat nystagmus with its fast phase in the direction of gaze (“direction-changing jerk nystagmus”) is the most common form of nystagmus; it may be congenital, caused by an acquired lesion of the brainstem, or reflect metabolic dysfunction, a paraneoplastic phenomenon, or medication toxicity
-
Tip: horizontal-rotary nystagmus with a fast phase that does not change directions in extremes of gaze (“non direction-changing”) and whose amplitude increases with gaze directed away from the side of the lesion suggests acute peripheral vestibulopathy; that diagnosis is fortified if acute vertigo, tinnitus, or hearing loss is present, and if there is no ataxia or skew deviation, and the head impulse test is positive
-
Tip: Wernicke encephalopathy can cause any form of nystagmus, but most typically sidebeat and upbeat jerk nystagmus; it should be suspected in any form of acquired nystagmus because treatment is effective and urgent!