( of )
Correct: 0
Incorrect: 0
A 38 year old woman complains of new headache and blurred vision in both eyes over the past week. In the emergency room, blood pressure is found to be 180/110 mm Hg. She has previously been normotensive and not known to have any systemic, neurologic, or ophthalmic issues. Visual acuities are 20/400 (6/120, 0.05) in each eye. There is no afferent pupil defect, intraocular pressures are normal, media are clear, and both optic fundi have the appearance seen in the left eye here.

What is causing the vision loss?
Incorrect
Correct!
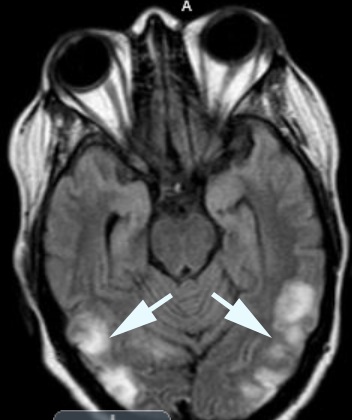 The abnormalities in the optic fundus—cotton wool spots, retinal hemorrhages, optic disc swelling—are the result of retinal vasospasm, microinfarction, and
vascular incompetence. But they do not account for the profound loss of vision. In acute systemic hypertension, the optic disc surface vessels often leak
and cause an engorged appearance of the discs, but the optic disc tissue is rarely infarcted. Instead, the vision loss comes from vascular leakage in the
occipital lobe white matter, where binocular profound vision loss can occur in a condition known as “posterior reversible encephalopathy syndrome” (PRES).
The abnormalities in the optic fundus—cotton wool spots, retinal hemorrhages, optic disc swelling—are the result of retinal vasospasm, microinfarction, and
vascular incompetence. But they do not account for the profound loss of vision. In acute systemic hypertension, the optic disc surface vessels often leak
and cause an engorged appearance of the discs, but the optic disc tissue is rarely infarcted. Instead, the vision loss comes from vascular leakage in the
occipital lobe white matter, where binocular profound vision loss can occur in a condition known as “posterior reversible encephalopathy syndrome” (PRES).
PRES occurs in two main settings: use of calcineurin inhibitors to prevent graft rejection or to treat intractable autoimmune phenomena, and in sudden
systemic hypertension, often during or after pregnancy.
If blood pressure is lowered, these abnormalities disappear rapidly and normal function is restored. But if there is a delay in lowering blood pressure, infarction may occur, leaving the patient with persistent retrogeniculate vision impairment. Tip: blood pressure must be lowered slowly to avoid ischemic optic neuropathy from acute systemic hypotension!
The optic fundus abnormalities—often dramatic—are a distraction. The real action is elsewhere and must be detected with brain imaging, preferably MRI. By the way, intracranial pressure is generally not much elevated in PRES. The minimal optic disc edema is the result of optic disc surface capillary leakage. Lumbar puncture is not indicated.
This patient had acute glomerulonephritis as the cause of elevated blood pressure.
If blood pressure is lowered, these abnormalities disappear rapidly and normal function is restored. But if there is a delay in lowering blood pressure, infarction may occur, leaving the patient with persistent retrogeniculate vision impairment. Tip: blood pressure must be lowered slowly to avoid ischemic optic neuropathy from acute systemic hypotension!
The optic fundus abnormalities—often dramatic—are a distraction. The real action is elsewhere and must be detected with brain imaging, preferably MRI. By the way, intracranial pressure is generally not much elevated in PRES. The minimal optic disc edema is the result of optic disc surface capillary leakage. Lumbar puncture is not indicated.
This patient had acute glomerulonephritis as the cause of elevated blood pressure.