( of )
Correct: 0
Incorrect: 0
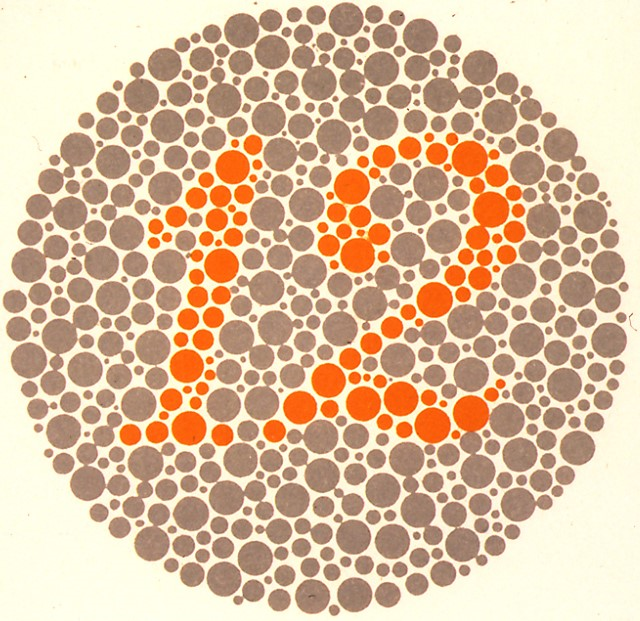
24 year old man reports gradually losing vision in both eyes and being bothered by ambient light. Your examination shows a visual acuity of 20/30 (6/9, 0.6) in both eyes with normal pupil size and constriction to light, full confrontation visual fields, and a normal-appearing optic fundus. With either eye being tested, he identifies only the Ishihara Pseudoisochromatic control plate (pictured here). Formal perimetry yields unreliable results.
What is the most likely cause for these abnormalities?
Incorrect
Incorrect
Correct!
You cannot be faulted for judging the sensitivity to light, impaired visual acuity and color vision, and unreliable formal visual field results as manifestations of a
psychogenic disorder. But organic causes could be at work! A bilateral optic neuropathy is not it because Ishihara color vision is too poor for this degree of visual
acuity loss. Congenital dyschromatopsia does not cause degraded visual acuity.
You must consider a diagnosis of photoreceptor dystrophy--even if the optic fundus examination appears normal, as it often does in that condition. You would settle the issue with an electroretinogram (ERG), which should show abnormalities in cone function (and often rod function). Optical coherence tomography might also show a disordered outer retina. The clinical manifestations can become apparent at any age. The lack of a family history should not dissuade you from the diagnosis. Sadly, visual acuity will gradually decline over time and there are yet no proven treatments. Two extremely rare conditions—autoimmune retinopathy and cancer-associated (paraneoplastic) retinopathy—should be excluded in the proper setting, but they are likely to produce constricted visual fields.
Diagnosis of those conditions depends on demonstrating anti-retinal antibodies in addition to the typical ERG abnormalities.
By the way, why is the patient bothered by sunshine? This symptom, called “hemeralopia,” results from the disordered cone function, which cannot normally transduce light into neural signals. Even normal-intensity light overloads the retina!
You must consider a diagnosis of photoreceptor dystrophy--even if the optic fundus examination appears normal, as it often does in that condition. You would settle the issue with an electroretinogram (ERG), which should show abnormalities in cone function (and often rod function). Optical coherence tomography might also show a disordered outer retina. The clinical manifestations can become apparent at any age. The lack of a family history should not dissuade you from the diagnosis. Sadly, visual acuity will gradually decline over time and there are yet no proven treatments. Two extremely rare conditions—autoimmune retinopathy and cancer-associated (paraneoplastic) retinopathy—should be excluded in the proper setting, but they are likely to produce constricted visual fields.
Diagnosis of those conditions depends on demonstrating anti-retinal antibodies in addition to the typical ERG abnormalities.
By the way, why is the patient bothered by sunshine? This symptom, called “hemeralopia,” results from the disordered cone function, which cannot normally transduce light into neural signals. Even normal-intensity light overloads the retina!
Incorrect