Orbital Myositis
- Autoimmune inflammation of extraocular muscles
- Considered a variant of orbital inflammation that may also involve the lacrimal gland, sclera, optic nerve sheath, periorbita, Tenon’s capsule, orbital fat
- Common causes: idiopathic (“idiopathic orbital inflammation”), sarcoidosis, systemic connective tissue disease
- Uncommon causes: IGG4 disease, granulomatous polyangiitis, giant cell arteritis, fungal sino-orbital infection
-
Core clinical features
- Periocular pain
- Diplopia
- Reduced ocular ductions
- Ocular misalignment
- Ptosis
- Proptosis
- Resistance to retropulsion of eye
- Eye tenderness
- Eyelid edema
- Episcleral hyperemia over extraocular muscle insertions
- Conjunctival hyperemia, chemosis
-
Possible accompanying clinical features
- Keratitis
- Scleritis
- Dacryoadenitis
- Uveitis
-
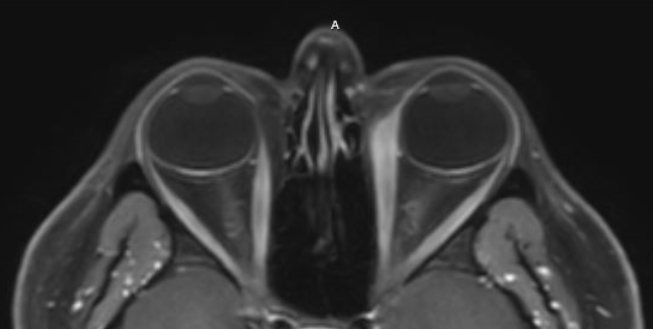
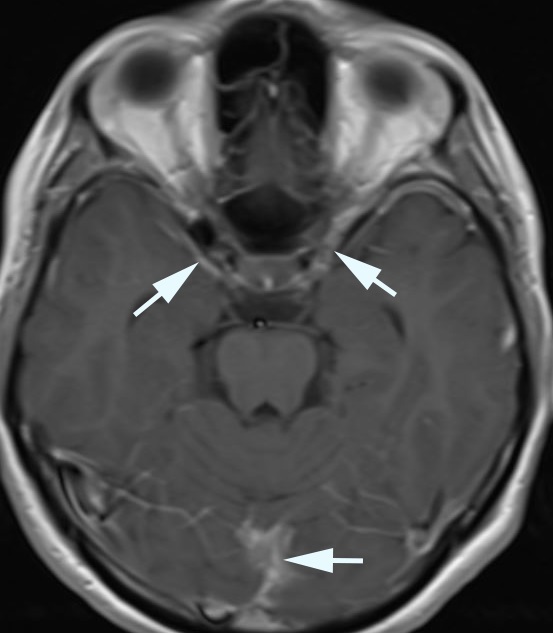
Imaging features
- Orbital imaging may show enlargement of extraocular muscles, enlargement of lacrimal gland, enhancement of dura, and congestion of orbital fat (“fat stranding”) and sinus mucosa, and rarely necrosis of muscle, mucosa, and bone
-
Trap: imaging may show normal or even small extraocular muscles when the disease has entered the atrophic phase
- Brain imaging may show pachymeningeal thickening and enhancement
- Body imaging may show pulmonary, serosal, or nodal abnormalities

- Graves disease
- Orbital infection (cellulitis, abscess)
- Orbital tumor
- Dacryocystitis (infected lacrimal sac)
- Severe viral or bacterial conjunctivitis
- Cavernous sinus fistula, thrombosis, tumor, inflammation
- Occult orbital trauma
-
Trap: fungal sino-orbital disease and necrotizing granulomatous polyangiitis may progress rapidly and need urgent treatment
-
Trap: bisphosphonates are often overlooked as a cause of ocular-orbital inflammation
- Evaluate for tenderness and resistance to retropulsion of the eye
- Perform forced (passive) ductions if large ductional deficits are present
- Perform orbital/brain imaging
-
Tip: MRI provides better definition of soft tissues, but CT is more available and better for bone
- Treat for orbital infection if that diagnosis cannot be safely excluded
- Pay special attention to excluding fungal sino-orbital disease in diabetes and other immune-compromised states
- Consider body imaging and blood tests if there are suggestive manifestations of a systemic process
- If infection has been excluded, treat empirically with prednisone 1mg/kg/day
- If manifestations improve with prednisone treatment, taper the prednisone dose slowly
- If manifestations recur, consider orbital biopsy if there is a discrete lesion
- If biopsy suggests inflammation, raise the prednisone dose
-
Trap: complications are bound to occur with long term use of corticosteroids
- Replace corticosteroids with a corticosteroid-sparing agent (azathioprine, methotrexate, cyclosporine, mycophenolate) if long-term treatment is required
- If treatment does not work, the myositis may have entered a cicatricial (scarred) phase or the diagnosis is incorrect
-
Trap: corticosteroid dependency does not exclude a neoplastic disorder
-
Trap: Patients with diffuse orbital imaging abnormalities are often misdiagnosed as having orbital cellulitis and treated with antibiotics, delaying anti-inflammatory treatment
- Prednisone treatment usually rapidly reduces active inflammation, but…
-
Trap: reactivation of inflammation is common, especially if the prednisone dose is tapered too rapidly
-
Tip: because corticosteroid dependency is common and potentially dangerous, replace corticosteroids with “corticosteroid-sparing” agents within weeks of starting treatment
- Inflammation usually “burns out” after months to years, but may leave eyes misaligned from scarred, shortened extraocular muscles
- Systemic autoimmune condition may be present at diagnosis or appear later
- Spectacle prisms may relieve diplopia in the short term, but an occluder of one eye, including an opaque contact lens, may be necessary
- Eye muscle surgery, which should be deferred until the condition is inactive, may relieve diplopia